Imagine your immune system as a vigilant security team, always on patrol to protect your body from intruders like viruses and harmful bacteria. But what happens when this security team gets confused and starts attacking your own home instead of the real threat? That, in essence, is what an autoimmune disease is.
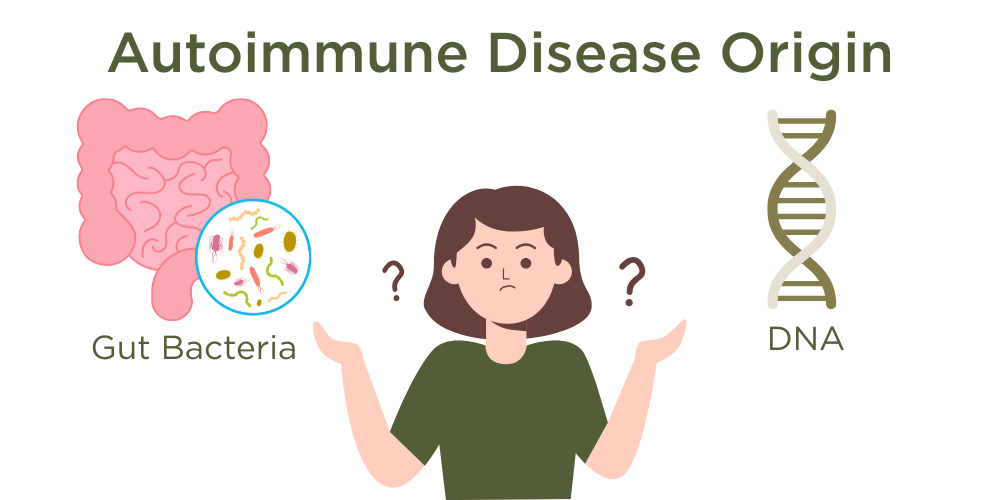
Autoimmune diseases occur when the immune system mistakenly targets the body’s own cells, tissues, and organs as if they were dangerous invaders. These conditions can arise for a couple of main reasons: inherited genetic factors or environmental triggers. Imbalances in the gut microbiome can bring on 80% of known autoimmune symptoms.
Understanding Autoimmune Disease Origins
1. Hereditary Factors
The blueprint of your body, known as your DNA, is inherited from your mother and father. It quietly dictates many things about you, including your risk of developing an autoimmune disease. Conditions like Psoriasis or Type 1 Diabetes can run in families, often linked to specific genes like HLA (human leukocyte antigen). These genes play a key role in how your immune system distinguishes between your own cells and foreign ones.
When these genes are programmed a certain way, they can signal T cells (a type of white blood cell) to become overly reactive. It’s as if the security team is always on high alert, mistaking your own tissues for threats and calling in backup in the form of inflammation.
2. Dysbiosis
Think of your gut as a garden full of microorganisms that help digest food, regulate mood, and balance the immune system. When this ecosystem gets out of balance, a state known as dysbiosis, it can confuse the immune system. Certain gut bacteria might activate genes in susceptible people, triggering a flare-up of autoimmune symptoms.
The Chain Reaction of a Flare-Up
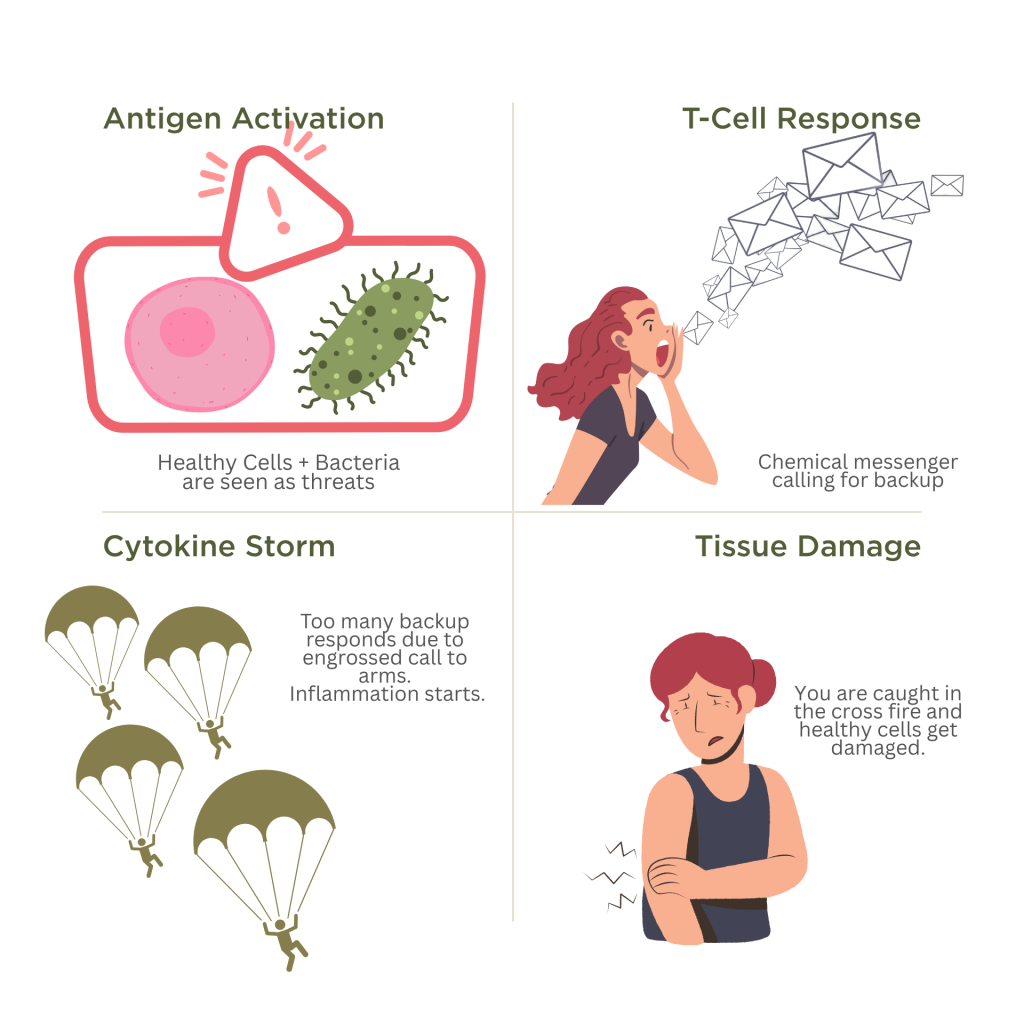
Genes are the building blocks of our DNA that codes everything about ourselves, from eye colour to our tastes, as well as how our immune system should function. Everyone has genes that respond to bacteria in different ways. In autoimmune patients, certain bacteria may trigger a response that sets off a cascade:
- Antigen Activation: An antigen is anything the body sees as a threat. In autoimmune diseases, the body misidentifies its own cells as antigens.
- T Cell Response: These white blood cells are activated and start releasing cytokines, which are chemical messengers.
- Cytokine Storm: These messengers call in more immune cells, creating inflammation.
- Tissue Damage: The healthy part of your body gets caught in the crossfire, leading to painful or disabling symptoms.
In Psoriasis, for example, this causes the skin cells (keratinocytes) to grow and multiply far too quickly. Imagine layers of skin piling up rapidly, forming red, itchy plaques.
Shared Mechanisms Across Autoimmune Diseases
Although they target different parts of the body, autoimmune diseases like Rheumatoid Arthritis, Lupus, IBS, MS, Guillain-Barré Syndrome, Psoriasis, Graves’ Disease, Hashimoto’s Thyroiditis, Scleroderma, Vasculitis, Type 1 Diabetes, and Myasthenia Gravis all work through similar mechanisms:
- Overactivation of T cells
- Cytokine-induced inflammation
- Mistaken identity of healthy cells as threats
For example:
- Rheumatoid Arthritis: T cells attack joint linings
- Lupus: Immune complexes form, attacking organs
- MS: Nerve coverings are destroyed
- Guillain-Barré: Nerves in the peripheral nervous system are targeted
- Type 1 Diabetes: Insulin-producing cells in the pancreas are destroyed
- Myasthenia Gravis: Immune response interferes with communication between nerves and muscles
Because these diseases follow a shared blueprint, they may also benefit from similar treatment strategies.
Holistic Approaches and Natural Remedies
Emerging research supports the role of certain herbs and natural compounds in calming the overactive immune system:
- Arctium lappa (Burdock Root): Helps rebalance immune responses and restore natural immune rhythm.
- Berberis aristata (Indian Barberry): Contains alkaloids that may dampen T cell activity, easing inflammation.
- Coleus forskohlii: Supports healthy cell turnover, helping the body replace damaged tissue.
- Coptis chinensis (Chinese Goldthread): Reduces T cell overactivity and calms overgrowth of skin cells, particularly useful in conditions like Psoriasis.
- Resveratrol: Found in grapes and berries, this compound has powerful anti-inflammatory effects that may slow down abnormal cell growth.
One standout natural solution is Fulvic Acid, which acts like a detoxifier, antioxidant, and immune modulator. Research shows it can improve inflammatory skin conditions by reducing cytokine production and calming flare-ups.
Vitamin D and Tulsi: Everyday Allies
- Vitamin D: Known as the “sunshine vitamin,” helps regulate T cell function. Deficiencies are linked with many autoimmune conditions, and restoring levels may improve outcomes.
- Tulsi (Holy Basil): Revered in Ayurvedic medicine, Tulsi acts as an adaptogen, helping the body manage stress while modulating immune responses and lowering inflammation through increasing serotonin and melatonin production.
Products such as Derma Balance Capsules and the Derma Balance Cream (for skin related reactions) incorporate these herbs to function synergistically.
Incorporating these natural strategies can be empowering but always consult a healthcare provider before making changes to your treatment plan. The goal is harmony within the immune system and across the body, not a battle.
When we understand what our bodies are trying to tell us, we can start manipulating the body’s natural mechanisms to that of healing, balance, and resilience.
Derma Balance Capsules
60 Capsules

